What Is KPV Peptide?
KPV functions as a competitive inhibitor of the IL-1β signaling pathway. By binding to the interleukin-1 receptor type 1 (IL-1R1) and preventing the recruitment of the accessory protein IL-1RAcP, it effectively blocks downstream activation of nuclear factor kappa B (NF-κB) and mitogen-activated protein kinases (MAPKs). This interference reduces transcription of pro-inflammatory cytokines such as tumor necrosis factor-α, interleukin-6 and chemokines that recruit neutrophils. Unlike broad-spectrum anti-inflammatories, KPV does not suppress the entire innate immune response; it selectively dampens IL-1β–driven inflammation while preserving essential antimicrobial functions.
Potent Anti-Inflammatory Effects
In vitro studies have demonstrated that nanomolar concentrations of KPV can inhibit neutrophil migration and reduce elastase release. In animal models of acute lung injury, intratracheal administration of KPV markedly decreased pulmonary edema, neutrophil infiltration and levels of IL-1β in bronchoalveolar lavage fluid. Similar protective effects were observed in a murine model of colitis where oral delivery of KPV lowered colon weight-to-length ratio, mucosal damage scores, and expression of inflammatory markers.
Beyond infectious or sterile inflammation, https://skitterphoto.com/photographers/1616210/booker-due KPV shows promise in chronic conditions such as rheumatoid arthritis and periodontitis. In collagen-induced arthritis models, systemic KPV administration reduced joint swelling and cartilage degradation while preserving normal bone remodeling. In periodontal disease models, topical application of KPV gel limited alveolar bone loss and maintained gingival tissue integrity.
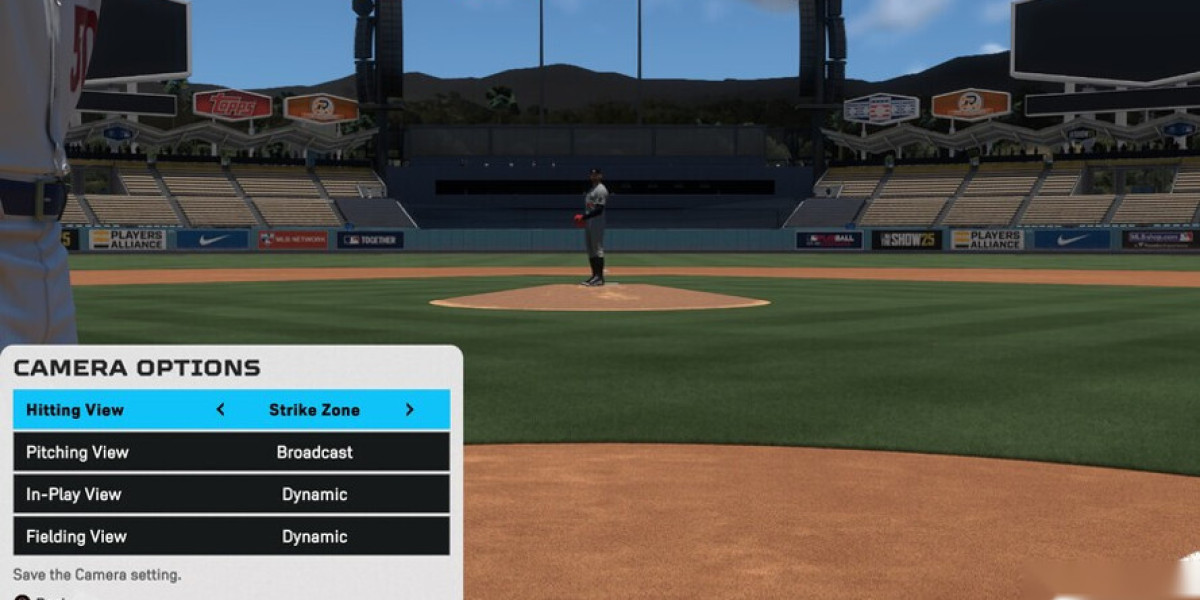
The peptide’s anti-inflammatory potency is further underscored by its pharmacokinetic profile: KPV is stable in serum for several hours, can be delivered via inhalation, oral tablets or transdermal patches, and exhibits minimal off-target effects. Its low immunogenicity allows repeated dosing without the risk of antibody neutralization.
Clinical Translation
Early phase clinical trials have explored KPV’s safety and efficacy in patients with asthma and chronic obstructive pulmonary disease (COPD). A double-blind, placebo-controlled study administering inhaled KPV reported significant reductions in sputum neutrophil counts and improvements in forced expiratory volume after 12 weeks. In a pilot trial for ulcerative colitis, oral KPV capsules reduced endoscopic scores and normalized fecal calprotectin levels.
Ongoing research aims to optimize delivery systems, such as nanoparticle encapsulation for targeted release at inflamed sites, and to investigate combinatorial use with conventional disease-modifying drugs. Preliminary data suggest that KPV can synergize with biologics targeting tumor necrosis factor-α or interleukin-6, potentially lowering required dosages of those agents.
Safety Considerations
Adverse event reports have been rare and mild, typically limited to transient injection site discomfort when administered parenterally. No significant alterations in complete blood counts, liver enzymes or renal function were observed in the trials conducted to date. The peptide’s specificity for IL-1R1 reduces the likelihood of systemic immunosuppression, a common drawback of many anti-inflammatory therapies.
Future Directions
Researchers are exploring KPV analogues with improved potency and resistance to proteolytic degradation. Structural modifications, such as cyclization or incorporation of D-amino acids, have yielded derivatives that retain receptor affinity while extending half-life in vivo. Additionally, investigations into the peptide’s role in neuroinflammation suggest potential applications in conditions like multiple sclerosis and traumatic brain injury.
In summary, KPV is a tripeptide with a well-defined mechanism of action targeting IL-1β signaling. Its potent anti-inflammatory effects across diverse disease models, coupled with a favorable safety profile and versatile delivery options, position it as a promising candidate for next-generation therapeutics aimed at controlling inflammation while preserving essential immune functions.